Two-thirds of COVID vaccines still unused in US: Surgeon General warns US needs to do a better
The Surgeon General has called on US states to relax their guidelines in order to get more Americans vaccinated as thousands of Florida seniors camped out in their cars overnight to get their shots and New York threatened to fine hospitals for not using up supplies amid a train wreck vaccine rollout across the country.
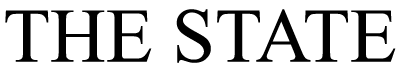
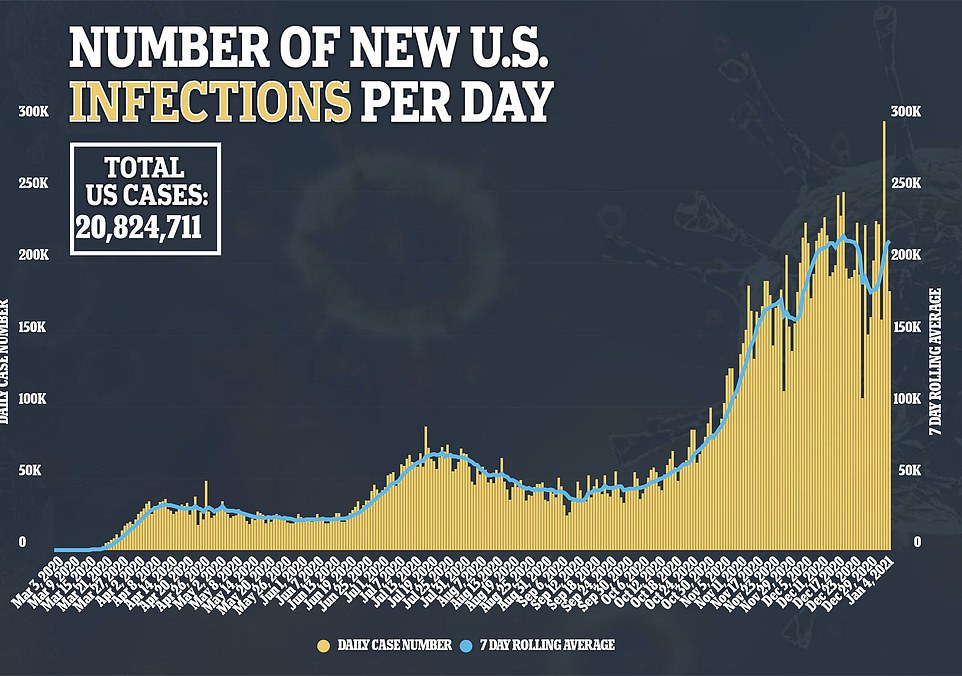
Just 4.66 million COVID-19 vaccines have been administered across the US in the last three weeks despite federal officials having distributed 15.4 million doses to the states. It means more than two-thirds of the vaccines shipped within the US have gone unused and just 1.4 percent of the population has been vaccinated even as cases, deaths and hospitalizations continue to surge across the US.
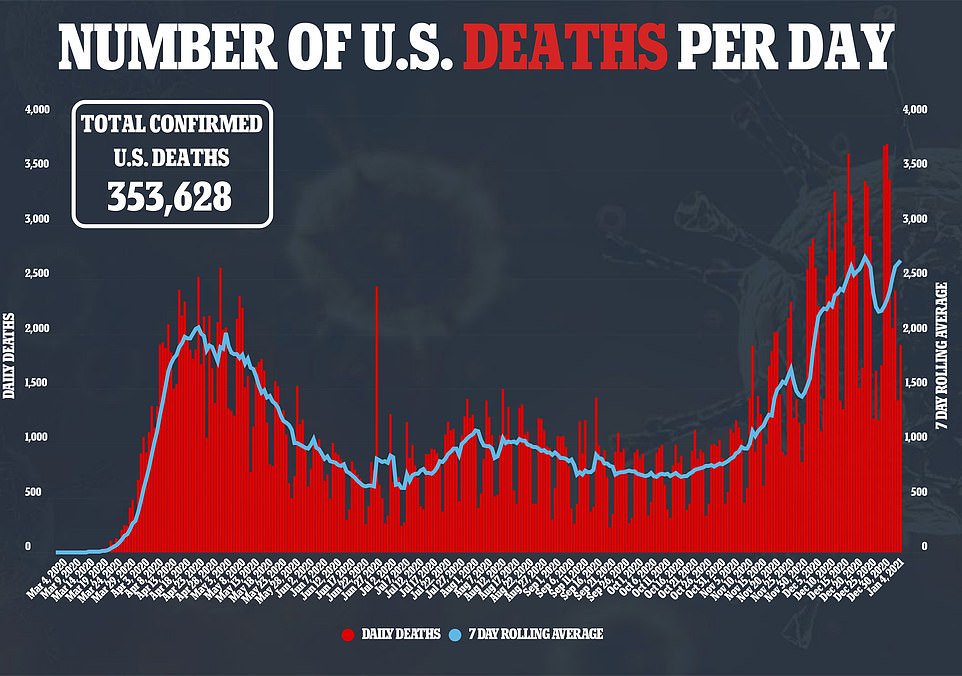
One in 930 Americans have now died from COVID-19 with the death toll surging past 353,000 and the seven-day rolling average for fatalities at just over 2,600 per day. There were 180,477 new infections across the country on Monday and a record 128,210 patients currently being treated for coronavirus in hospitals.
Surgeon General Jerome Adams on Tuesday admitted that the largest vaccination campaign in US history, which has been in the works for months, has been a ‘little bit messy’.
He blamed, in part, the states for the slower than expected rollout and called on governors to speed up the process by moving to the next priority groups if demand wasn’t being met.
Based on guidelines issued by the federal government, most states are currently prioritizing frontline healthworkers and nursing home residents in the first phase, before moving on to the elderly and other essential workers.
‘In many cases, (the vaccines) are sitting in freezers. We’ve been telling these states since September, we need to prioritize getting everyone vaccinated as quickly as possible while trying to adhere to the guidelines,’ Adams told NBC’s Today. ‘If healthcare workers don’t want to get these vaccines in some places… we need to move on to the (next groups).
‘If the demand isn’t there in 1A, go to 1B and continue on down. If the demand isn’t there in one location, move those vaccines to another location.’

FLORIDA: Hundreds of seniors camped up in their cars overnight on Monday in Daytona Beach, Florida parking lot in order to get their first dose of the vaccine. In Florida, where officials have put senior citizens ahead of many essential workers for getting the vaccine. Image courtesy of NBC

FLORIDA: Hundreds of seniors camped out overnight at Daytona Beach Municipal Stadium to be first in line for vaccinations in the state
Just 4.66 million COVID-19 vaccines have been administered across the US in the last three weeks despite federal officials having distributed 15.4 million doses to the states
In other COVID-19 vaccine news:
- Hard-hit California has only vaccinated 1 percent of its 40 million population
- Governors of New York and Florida have vowed to penalize hospitals that fail to dispense shots quickly
- New York City Mayor Bill de Blasio says the city’s hospitals vaccinated just 148 people across the five boroughs on January 1 – delivering just 13 doses per hospital
- According to a state-by-state breakdown, Kansas and Georgia have only administered 17 percent of the doses distributed to them
- Most states are prioritizing healthcare workers in hospitals for phase one but Florida is allowing senior citizens to be among the first vaccinated
The widespread rollout failures have already been blamed on a range of factors, including governors setting convoluted priorities for initial distribution, lack of federal oversight, chaos in distribution given the freezing temperatures of the Pfizer and Moderna vaccines, and the simple lack of staff to administer jabs in overstretched healthcare systems.
Surgeon General Jerome Adams on Tuesday admitted that the largest vaccination campaign in US history, which has been in the works for months amid the pandemic, has been a ‘little bit messy’
Adams warned the US needed to do a better job of matching up supply and demand in states like Florida where hundreds of seniors camped out in their cars overnight in Daytona Beach in order to get their shots.
The seniors camped out in the Daytona Stadium parking lot so they could be first in line for at the drive-thru vaccine facility. In other parts of Florida, seniors are registering online to get access to the shots.
‘The problem is we need to do a better job of matching up supply and demand at the local level,’ Adams said.
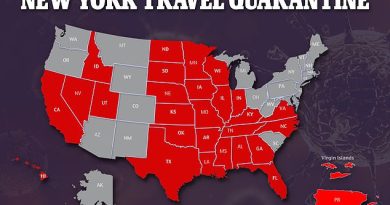
‘Some states are doing a really good job. You have red states like North and South Dakota and blue places like DC and Connecticut who have distributed 75 plus percent of their vaccines. But you have some states that still haven’t distributed 25 percent of their vaccines.’
The race to vaccinate Americans quickly comes as a super-contagious mutant strain of COVID-19 that has forced the UK into its third lockdown has already been detected in the US. Ten people, who are spread across New York, California, Colorado and Florida, have been confirmed to have the variant of the virus. British Prime Minister Boris Johnson has revealed that one in 50 in England – around a million people all up – are now infected with coronavirus.
According to a state-by-state breakdown, Kansas and Georgia have only administered 17 percent of the doses distributed to them. Hard-hit California has so far used 24 percent of its vaccine shots, while Florida has used 23 percent. New York, the initial epicenter of the outbreak, has used up 33 percent of its allocation.
Only a handful of states have used more than 50 percent of the shots distributed to them: South Dakota (62%), North Dakota (58%), Tennessee (50%), Connecticut (50%) and Maine (50%).
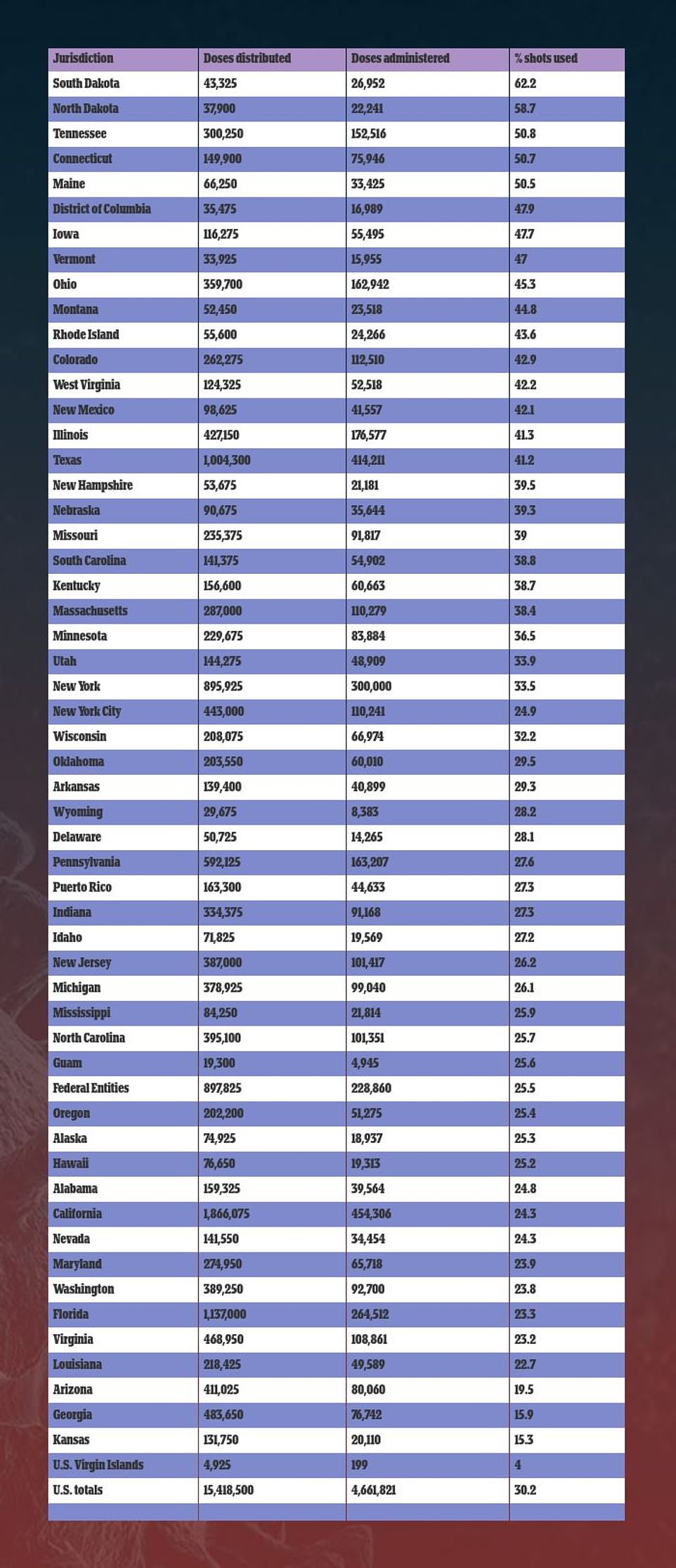
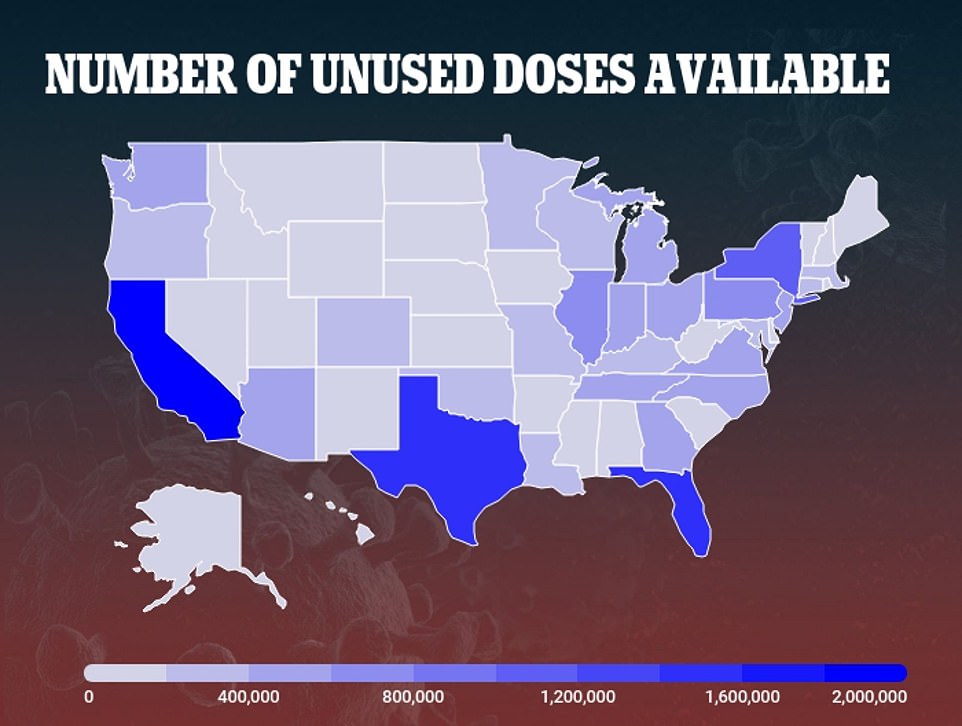
According to a state-by-state breakdown, Kansas and Georgia have only administered 17 percent of the doses distributed to them. Hard-hit California has so far used 24 percent of its vaccine shots, while Florida has used 23 percent
California Gov Gavin Newsom said on Monday that his state has only vaccinated 1 percent of the population.
He said distribution hiccups and logistical challenges have slowed the initial vaccine rollout in California, setting a pace that he said is ‘not good enough’.
The 454,000 doses of vaccine that have been administered in California represent just a third of the more than nearly 1.3 million received in the state so far, according to the California Department of Public Health.
Even as he acknowledged the state must do better, Newsom sought to shift some responsibility for the slow rollout, noting ‘the vaccines don’t arrive magically in some state facility.’
The governors of New York and Florida have already vowed to penalize hospitals that fail to dispense shots quickly.
In New York, hospitals must administer vaccines within a week of receiving them or face a fine and a reduction in future supplies, Gov Andrew Cuomo said, just hours before announcing the state’s first known case of a new, more infectious coronavirus variant originally detected in Britain.
‘I don’t want the vaccine in a fridge or a freezer, I want it in somebody’s arm,’ Cuomo said. ‘If you’re not performing this function, it does raise questions about the operating efficiency of the hospital.’
New York hospitals on the whole have dispensed fewer than half of their allocated doses to date, but performance varied from one group of hospitals to another.
The NYC Health + Hospitals system, the city’s main public hospital network, has only administered 31 percent of its allotment, compared with 99 percent for a few private hospitals in the state.
The CDC reported an even lower vaccine uptake for New York overall, saying fewer than one in five of the 896,000 doses shipped to the state since mid-December have been given.
New York City Mayor Bill de Blasio revealed on Monday that the city’s hospitals vaccinated just 148 people across the five boroughs on January 1 – delivering just 13 doses per hospital.
It came as he promised to vaccinate 100,000 people every week going forward.

FLORIDA: Hundreds of seniors and first responders wait in lin
e for a COVID-19 vaccine on Tuesday at Central Broward Park in Lauderhill

NEW YORK: A resident at Hamilton Park Nursing and Rehabilitation, a nursing home facility, receives the Pfizer vaccine from Walgreens pharmacists in Brooklyn on Monday

CALIFORNIA: Engineer/paramedic Bonnie Breckenridge (right), gives the the Pfizer vaccine to Fire Chief Colin Stowell (left) at the San Diego Fire-Rescue Training Facility
In Florida, where officials have put senior citizens ahead of many essential workers for getting the vaccine, Governor Ron DeSantis announced a policy under which the state would allocate more doses to hospitals that dispense them most quickly.
‘Hospitals that do not do a good job of getting the vaccine out will have their allocations transferred to hospitals that are doing a good job at getting the vaccine out,’ DeSantis said.
‘We do not want vaccine to just be idle at some hospital system,’ he added, although he did not say they would face fines.
Florida, which has dispensed less than a quarter of the 1.14 million doses it has received, according to the CDC, will also deploy an additional 1,000 nurses to administer vaccines and will keep state-run vaccination sites open seven days a week, DeSantis said.
In Florida, in particular, elderly residents have said they are unsure how to even access the vaccine – even though they are being prioritized.
Some counties have set up online portals or phone lines so elderly residents can sign up for vaccinations but multiple local health departments reported crashing systems on Monday.
Dr Amesh Adalja, a scholar at the Johns Hopkins Center for Health Security, said New York and Florida were being ‘overly bureaucratic’ in penalizing hospitals over vaccine deliveries even as they coped with soaring patient caseloads.
‘Instead of fining hospitals, why not give them more resources to do this, more money, more staffing?’ he said.
Pennsylvania’s Health Secretary Dr Rachel Levine has blamed the holiday period for their slow rollout. The state has so far administered 163,207 of its allocated 592,125 doses.
‘I think it was always going to be a challenge during those two to three weeks to administer the shots that were sent to us,’ Levine said.
Across the country, the pace of immunizations has gone slower than planned due to logistical hurdles and differing approaches across states and counties.
The failure to speedily vaccinate millions of Americans has already been blamed on various factors, including lack of federal oversights and chaotic distribution.
The 20 million-dose goal hasn’t been reached in part because local health departments and medical facilities had to stay focused on testing to handle a surge in cases, the Surgeon General has previously said, adding that the holiday season meant health workers were taking time off.
Medical authorities have confronted widespread distrust of immunization safety, even among some healthcare workers, owing in part to the record speed with which COVID-19 vaccines were developed and approved 11 months after the virus emerged in the US.
But some officials also have cited organizational glitches in launching the most ambitious mass inoculation campaign in the nation’s history in the year-end holiday season.
‘The logistics of getting it going into the people who want it is really the issue,’ Dr Anthony Fauci, told MSNBC. ‘We’re not where we want to be. No doubt about that. ‘I don’t think we can blame it all on vaccine hesitancy.’

CASES PER CAPITA: While the dire situation in California continues to unfold, Arizona is now currently the worst affected state for cases per capita with an average of 121 cases per 100,000 residents in the last seven days, according to the latest CDC data
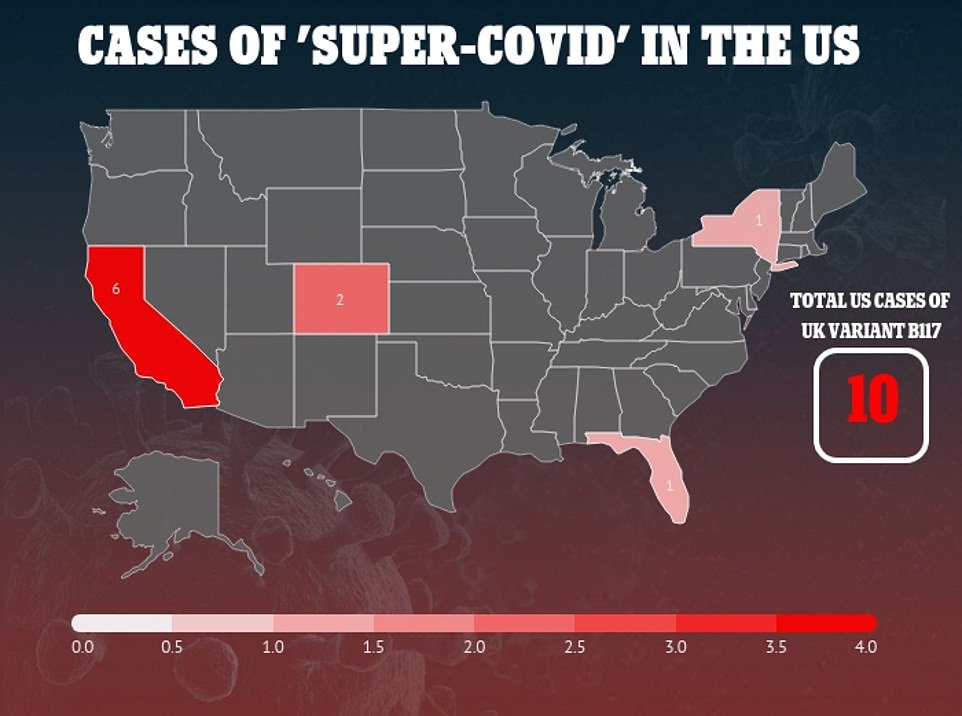
The race to vaccinate American quickly comes as a super-contagious mutant strain of COVID-19 that has forced the UK into its third lockdown has already been detected in the US. Ten people, who are spread across New York, California, Colorado and Florida, have been confirmed to have the variant of the virus
Give as many people one dose of coronavirus vaccine as possible, Ivy League experts say: Studies find a single shot is at least 50% effective and giving more first jabs is cheaper
Three new studies suggest that as many people as possible should receive at least one dose of the coronavirus vaccine.
Currently, both vaccines approved for emergency use authorization in the U.S. – from Pfizer Inc and Moderna Inc – require two doses administered about one month apart.
But researchers from Yale University, Stanford University and the University of Washington have found that an initial dose is about 50 percent effective at preventing COVID-19 infection.
This could help curb the spread of the virus and help relieve hospital systems from some of the strain they are under – and then second doses could be given a few months later.
The trio of new research, published in the Annals of Internal Medicine, suggest giving as many Americans as possible one dose of the COVID-19 vaccine before distributing the second dose could ‘maximize population health benefits.’
In one study, conducted by Stanford University, researchers developed a model to test different vaccine distribution methods.
The first model, known as the ‘fixed strategy,’ gives 50 percent of patients their first doses and reserved the other 50 percent for the second dose three weeks later.
The second model, known as the ‘flexible strategy,’ reserves 10 percent of the supply for second doses during the first three weeks, 90 percent during each of the next three weeks, and 50 percent thereafter.
Results showed the flexible strategy would result in preventing between 23 percent and 29 percent of cases COVID-19.
In both scenarios, 24 million people received at least one dose of the vaccine by week eight.
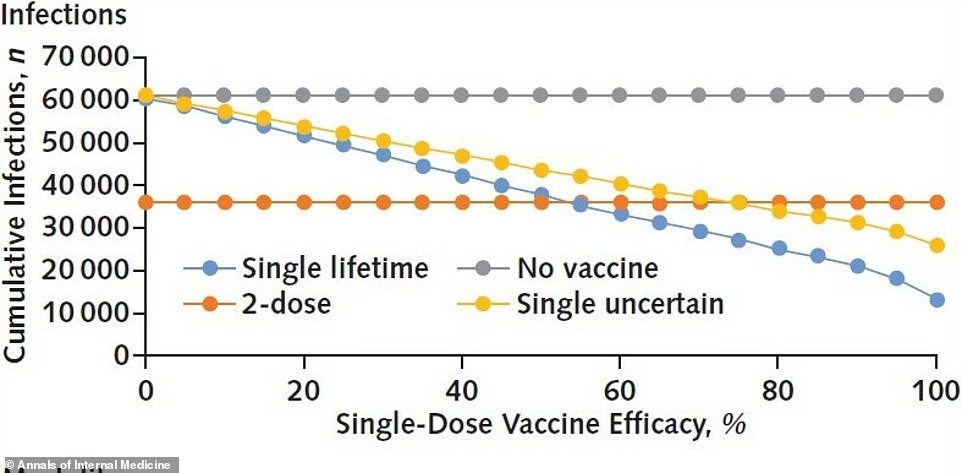
Studies from Yale University and the University of Washington found that one dose of the coronavirus vaccine (yellow and blue lines) is about 50% effective, which could help reduce the number of infections
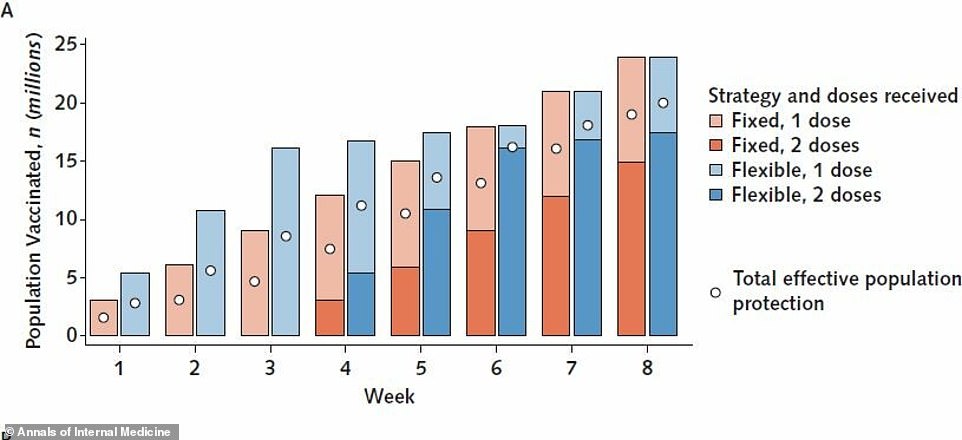
Another study, from Stanford University found that giving as many as people as possible a first dose, known as a ‘flexible strategy,’ could reduce an additional 23% to 29% of COVID-19
cases (above)
However, in the flexible strategy resulted in 2.4 million additional people receiving two doses because one million more people had been given an initial dose during the first three week compared to the other strategy.
‘We find that under most plausible scenarios, a more balanced approach that withholds fewer doses during early distribution in order to vaccinate more people as soon as possible could substantially increase the benefits of vaccines, while enabling most recipients to receive second doses on schedule,’ the authors wrote.
In another study, from Yale University, the team developed a model analyzing coronavirus transmission and vaccination leading to protective immunity.
Consistent with the Food and Drug Administration (FDA), researchers assumed the two-dose vaccine would prevent the risk of contracting the coronavirus by 95 percent and took four weeks to achieve lifetime protection.
This was compared with two hypothetical, single-dose alternatives, one with lifetime protection and the other with protection for about six months.
The model showed that a single-dose with six months of protection would need to be 75 percent effective to prevent as many infections as a two-dose vaccine with 95 percent efficacy.
However, a single-dose vaccine conferring lifetime protection would only need to be about 55 percent effective to avert as many infections as the two-dose jab.
‘The success of a COVID-19 vaccination program will depend more on the speed and reach of its implementation than on the efficacy of the vaccine itself,’ the authors wrote.
‘Depending on the duration of protection conferred, a single-dose vaccine with 55% effectiveness may confer greater population benefit than a 95%-effective vaccine requiring two doses.’
The third article, an editorial, from a team at the University of Washington and Fred Hutchinson Cancer Research Center, analyzed data from the clinical trials run by Pfizer-BioNTech and Moderna.
A single dose of the Pfizer-BioNTech shot was found to be 52 percent effective at preventing COVID-19 infection.
Meanwhile, the Moderna jab was reported to be 51 percent effective in the first 14 days after the first dose.
Additionally, a single dose of the Moderna vaccine decreased the number of asymptomatic coronavirus infections by two-thirds.
Based on these findings, they suggest that speed of the vaccine rollout is essential for controlling the COVID-19 pandemic rather than administering two doses.
‘Doubling the vaccine coverage with a single dose compared with a two-dose regimen will accelerate pandemic control because even lack of complete protection on an individual level is likely to lower transmission rates enough to stop epidemic growth,’ they wrote.
‘Providing effective protection for as many people as possible is more ethical because it distributes the scarce commodity more justly.’
The researchers also noted that more adverse events, such as fever, headache, fatigue and chills, were reported within seven days of people receiving the second dose compared to the first dose.
‘A single-dose vaccine approach could mitigate the higher incidence of many vaccine-associated adverse events seen with the second vaccine dose, increasing tolerability and thus likely acceptability in the general population,’ they wrote.