Coronavirus UK: 70,000 develop infection every day, app estimates
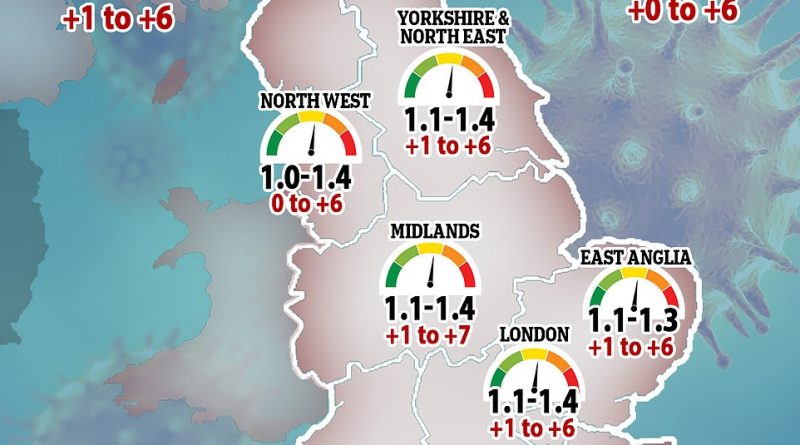
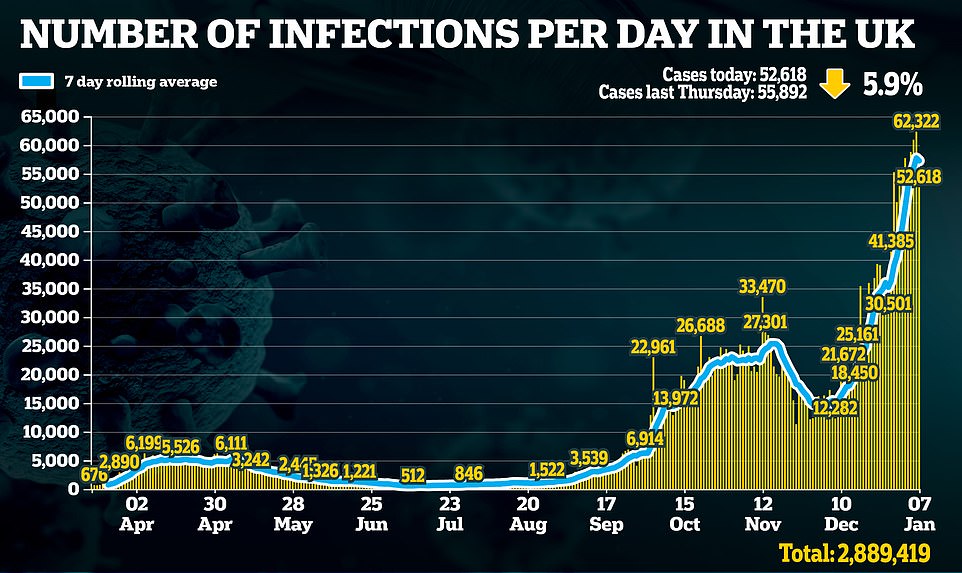
The coronavirus R rate in Britain could be anywhere between 1.0 and 1.4, SAGE said today as studies estimated that 70,000 people are catching the infection every day and the new variant accounts for 61 per cent of cases in England.
SAGE’s reproduction rate, which shows how many people each infected person passes the virus to, has been given a wider range than the estimated 1.1 to 1.3 last week, meaning scientists aren’t sure how fast the outbreak is growing – but they are certain it is not shrinking.
It was similar across all seven regions of England, and had only dropped in the areas that were under Tier 4 restrictions before Christmas – London, the South East and the East of England. It rose in all other regions.
The R rate was highest in the South West at 1.1 to 1.5, meaning the outbreak may be growing fastest there. In four regions – London, the Midlands, North East and Yorkshire and the South East – the R rate was at 1.1 to 1.4, in the East of England it was between 1.1 and 1.3 and in the North West it was 1.0 to 1.4.
It was not below one in any region, suggesting top scientists think England’s Covid outbreak is still growing in all areas despite the third lockdown being in place for four days. Experts say its impact won’t be clear for another two weeks, because it takes this long for someone who was infected with Covid-19 before the draconian measures came into force to develop symptoms and get a positive test result, impacting the R rate.
But they argue the nationwide shutdown will start bringing down the daily number of infections because of curbs on social interaction, which is what the virus relies on to spread between households.
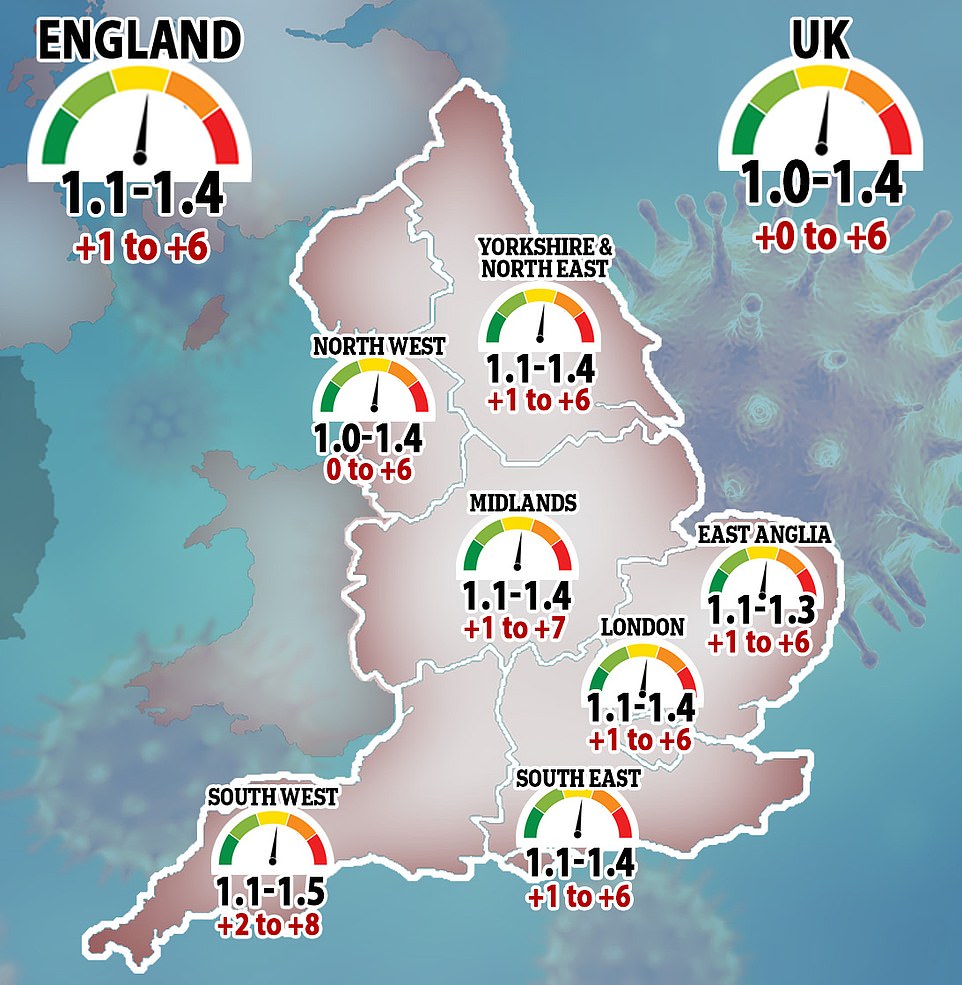
The team behind the ZOE Covid Symptom Study app, carried out with King’s College London, say the number of people reporting symptoms each day is up 27 per cent in a week from 55,226 to 69,958.
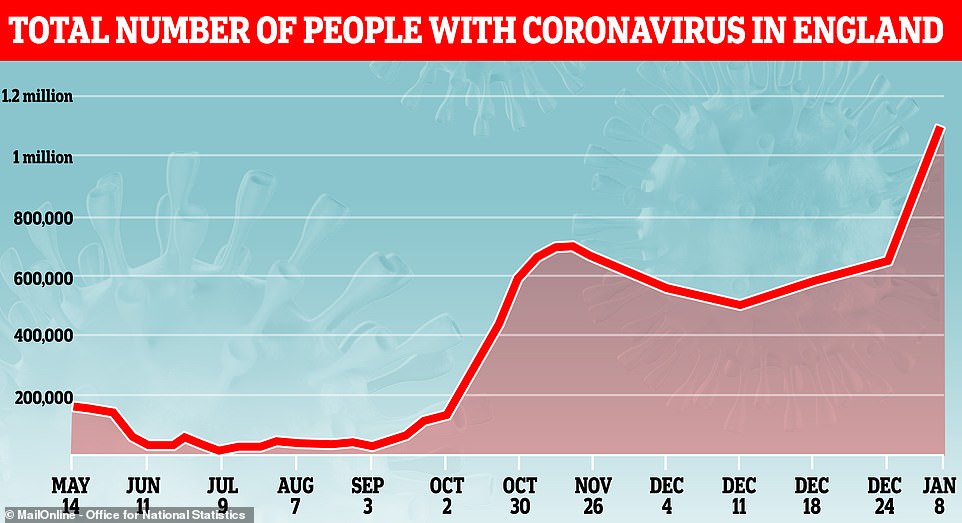
And separate research by the Office for National Statistics estimated that 1.1million people were infected with the coronavirus, and that almost two thirds of cases have the fast-spreading variant of the virus.
The variant has become dominant in some regions, found in 81 per cent of cases in London, but is still linked to fewer than half of infections in the North of England, the Midlands and Scotland, Wales and Northern Ireland.
Pfizer, the US company behind the first Covid vaccine to be approved in the UK which is now being given to millions of people, said today that it has tested the jab against the new variant and it appears to still work normally.
Despite infection numbers soaring across the UK, with England accounting for 57,157 of the daily cases in this week’s release, there are signs that infections are starting to come down in London, the ZOE researchers said. The capital remains the hotspot, with almost a quarter of all the UK’s infections (23 per cent), but has been in lockdown for three weeks after Tier 4 started on December 19 and ran into the national lockdown.
The staggering numbers add to evidence that the second wave is out of control, as Department of Health officials have announced more than 50,000 new positive tests every day for the last 10 days, meaning over half a million people have been diagnosed in less than a fortnight, and the true number of cases is likely to be far higher.
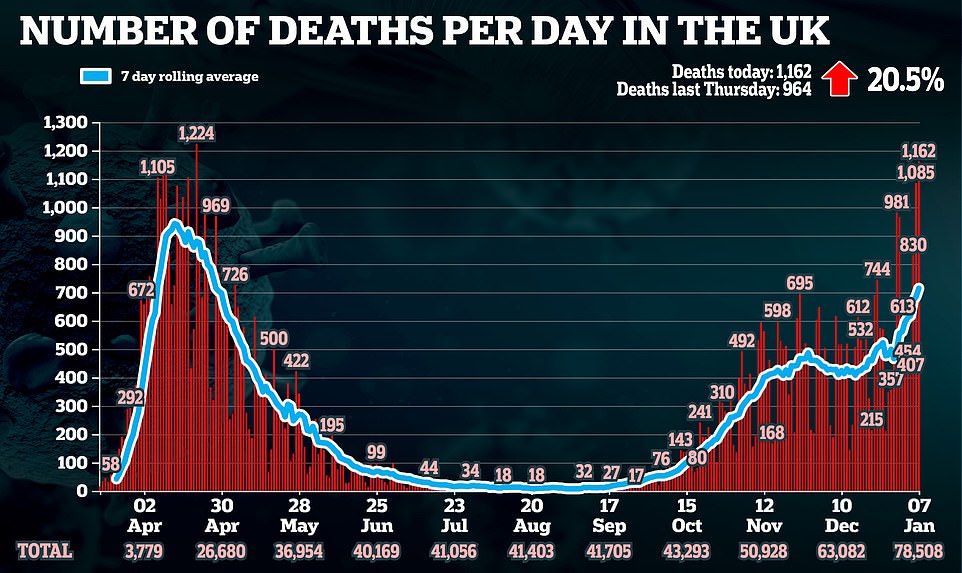
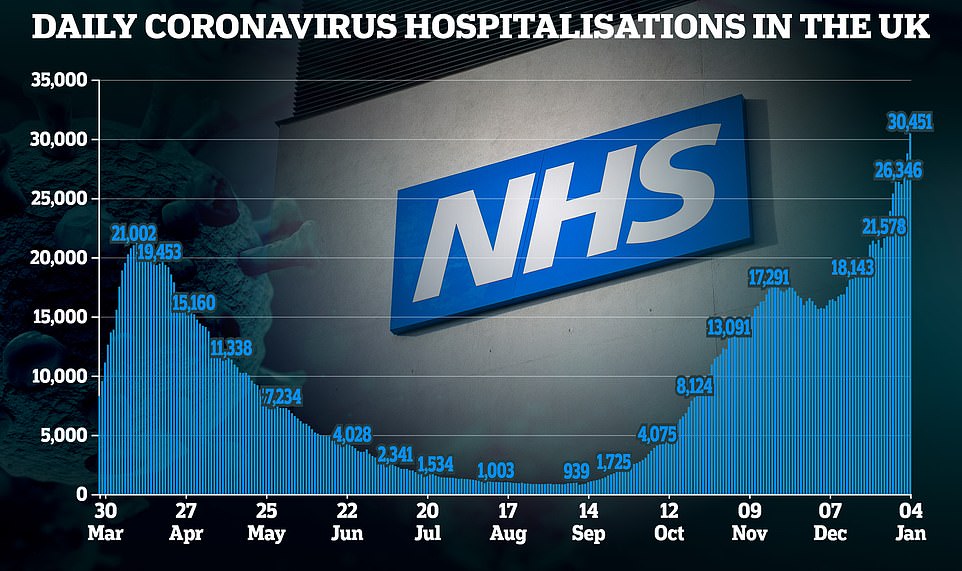
As an inevitable result of soaring cases, the number of hospital patients is now above 30,000 and higher than ever, and 1,162 deaths were announced yesterday – in Britain’s second worst daily death toll since the pandemic began.
England is now in its toughest and longest lockdown since last spring and may not emerge from it until all the most vulnerable groups have been vaccinated against Covid-19. The Government has ambitious plans to immunise 13.9m by mid-February and Boris Johnson claims it will be able to give 200,00 jabs a day by next week.
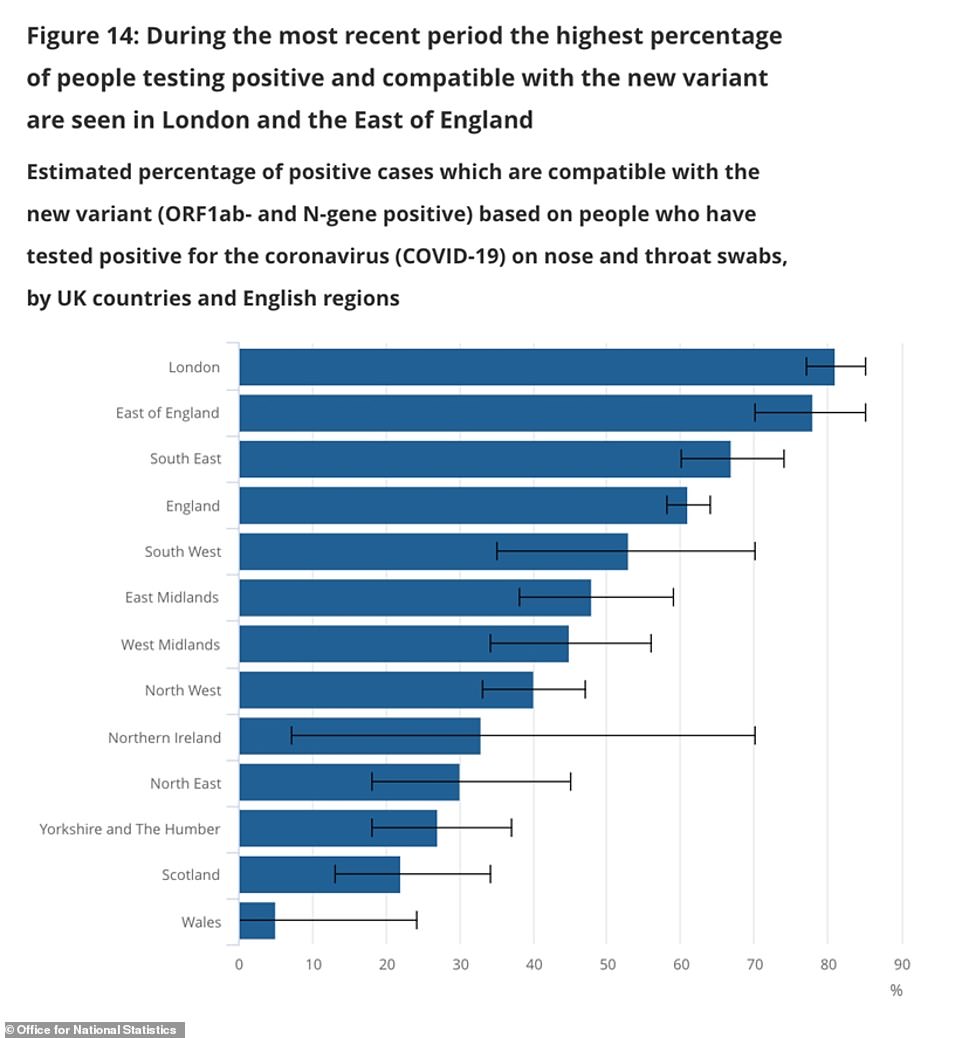
The Office for National Statistics found in its mass testing programme that almost two thirds (61%) of the positive tests it found in England appeared to be linked to the new variant of the virus. The figure was higher for some regions – particularly in London and the South – but lower in others
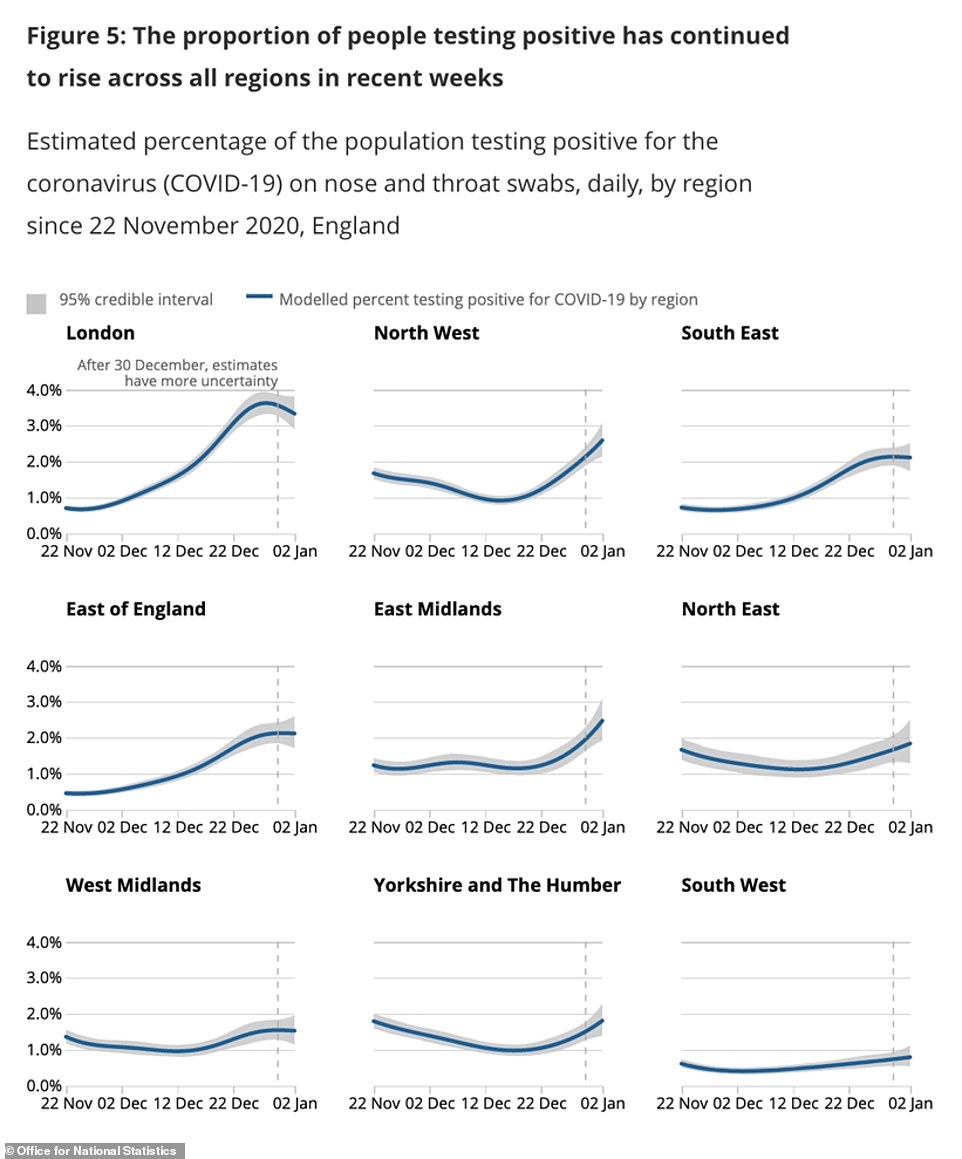
Positive cases appeared to be starting to fall or level off in London, the East and South East of England in this week’s ONS data, which Professor Christ Whitty picked up on in a press briefing earlier this week
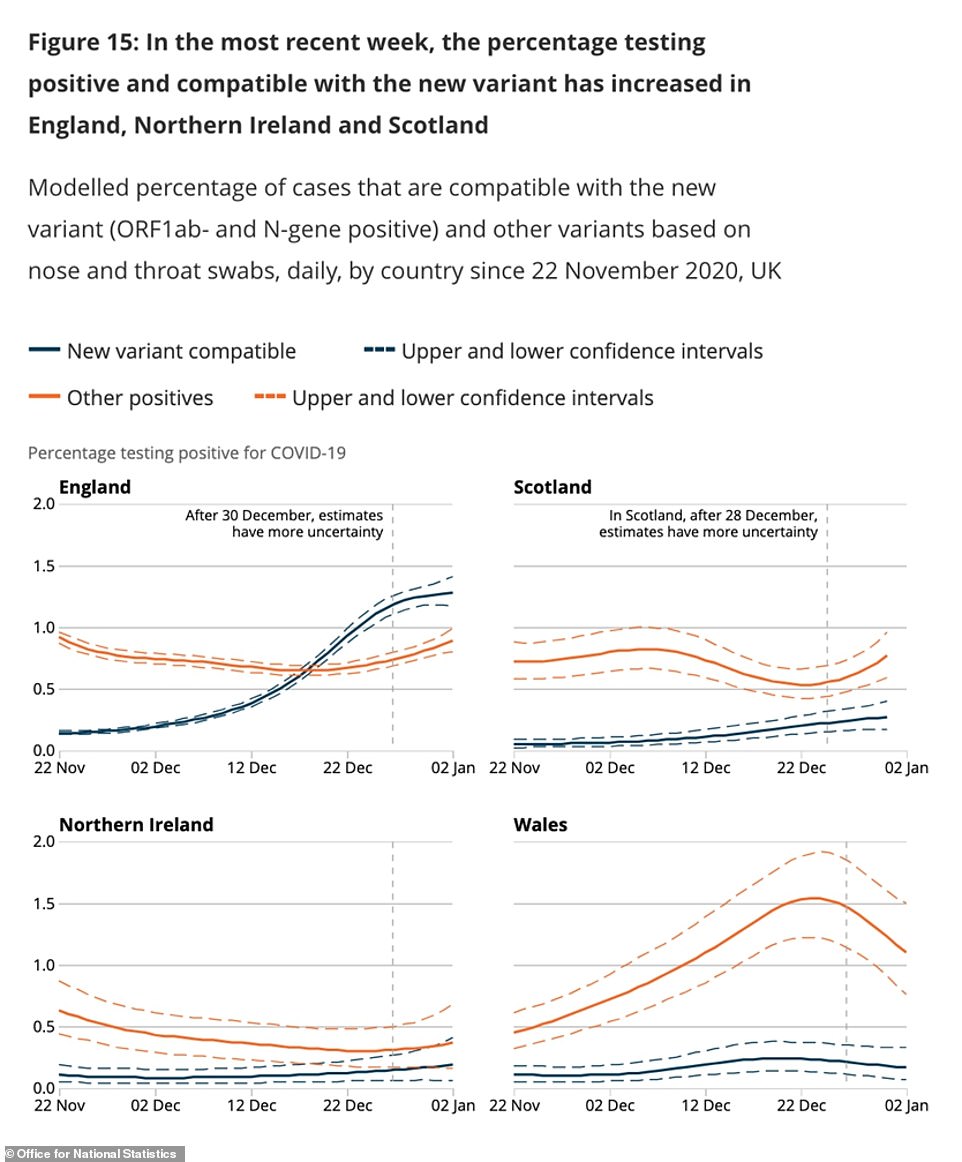
The new variant of coronavirus (blue line) has become the dominant strain in England but is not yet more common than other types of the virus in the UK’s other countries, Scotland, Wales and Northern Ireland, ONS testing shows
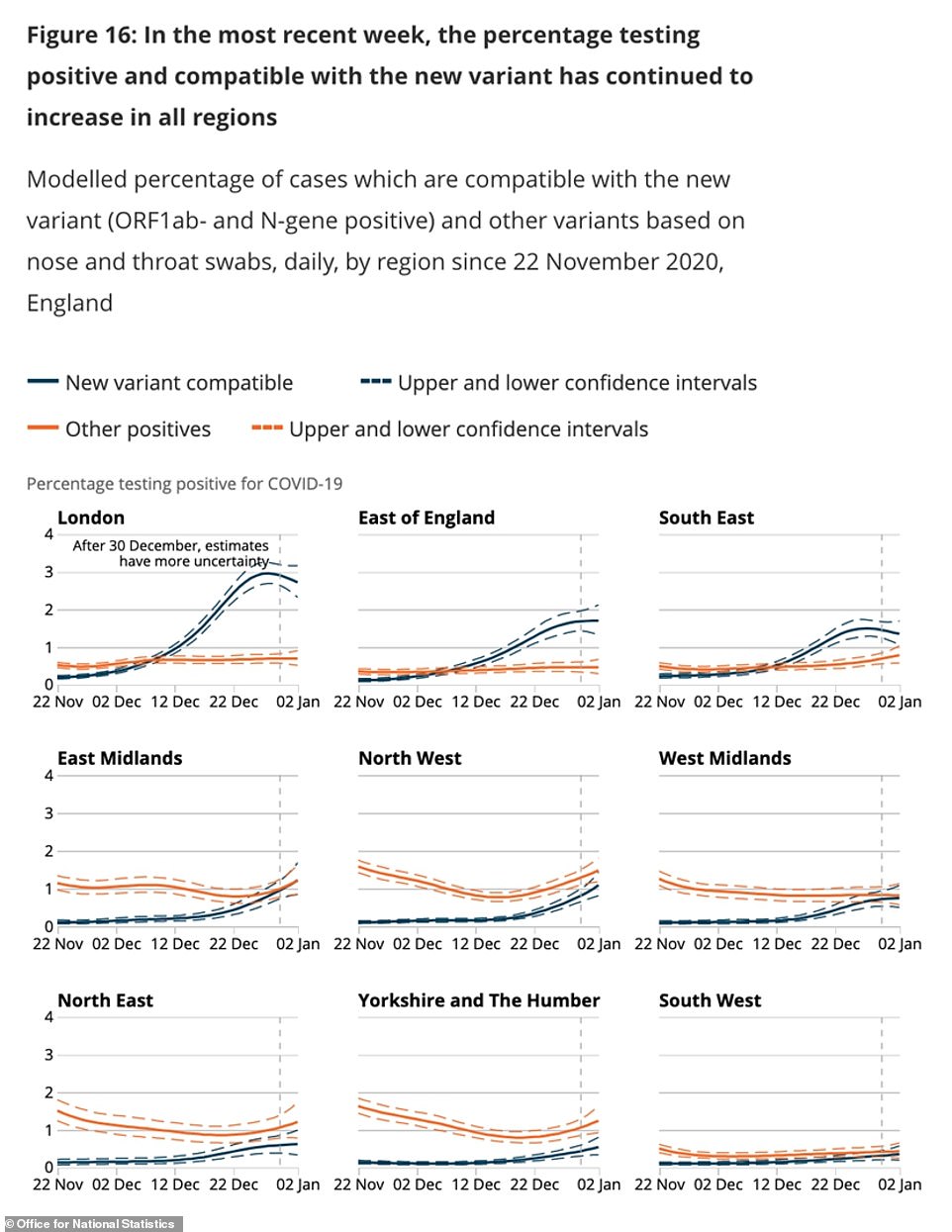
The Kent variant of the virus (blue line) has become dominant in London, the East of England and the South East, but not yet in other parts of the country, although it is narrowing the gap in most places
In their report today the ONS experts said their testing shows there has been a growth in the number of people testing positive for the new variant of the virus.
They can track this because the tests they use cannot detect the mutated gene in the new variant – meaning it only picks up on two out of the three main genetic targets it uses to spot coronavirus. This is called a ‘drop-out’ and, by looking at how many cases have this gene drop-out, they can calculate how many are linked to the variant.
The report said: ‘The highest percentages are seen in London, the East of England and the South East. In contrast, the percentages of cases compatible with the new variant remain relatively low in other regions at present.’
The ZOE and King’s team predict that the reproduction rate (R) of the virus is above one in all parts of the UK and that the outbreak is worst in London.
They estimate the R is 1.2, on average, across England and 1.0 in Wales and 1.3 in Scotland.
Professor Tim Spector, the King’s College epidemiologist leading the study, said today: ‘The UK is now worryingly at 70,000 new daily cases and around 800,000 infected individuals, and the worst hit areas continue to be Wales, London and the South East.
‘Our ZOE survey data is the most reliable source of the changing rates of infection over the holiday fortnight.
‘One in 42 people in London has symptomatic COVID now, so those living in the capital must take care. The good news is that we are now seeing new cases in London coming down slightly.
‘These figures are from the 3rd of January suggesting numbers had started to fall just before the announcement of the English national lockdown.’
The numbers produced by the Covid Symptom Study are based on reports from a million regular
users of the mobile app, who log whether they feel ill as well as the results of any coronavirus tests they have taken.
It is unofficial but is the largest surveillance programme in the country, although it cannot estimate the number of people with coronavirus but without symptoms.
The data in this week’s report suggests that London is by far the worst affected region of the country, with an estimated 16,813 people getting symptomatic Covid-19 every day this week.
It was followed by the South East with 9,059 cases, the East of England with 7,856 and the Midlands with 7,403.
Infections were lowest in the South West, where there were 3,464 infections per day, and in North West. There were between 5,000 and 6,000 per day in each of Scotland, Wales, the North West and the North East and Yorkshire.
The Office for National Statistics, which uses mass testing to try and work out the true number of people infected with the coronavirus, is considered the most accurate measure of the true number of cases.
This picks up on infections whether people have symptoms or not, and this week estimated a staggering two per cent of the population has coronavirus – one in every 50 people. This rose as high as one in 30 in London.
Boris Johnson announced the shocking infection rate in a TV briefing on Tuesday, January 5, when he laid out plans for the UK’s third and, hopefully, final national lockdown.
The PM said the scorching spread of the mutant variant of the virus, which has caused case numbers to explode in London and the South East, meant there was ‘no choice’ about imposing lockdown.
But he insisted the measures can get the situation under control while vaccines are rolled out – revealing that 1.3million people have now had jabs as he dismissed criticism that he is ‘over-promising’ about the most vulnerable categories being covered by mid-February.
Mr Johnson vowed to give the country ‘jab by jab’ information about the crucial immunisation process, now seen as the only way out of the relentless cycle of lockdowns.
He was flanked at the press conference by medical and science chiefs Chris Whitty and Patrick Vallance, whose warnings about the threat of the NHS being overwhelmed sparked the extraordinary U-turn to plunge England into new restrictions.
The podiums once again were adorned with the slogan from March 2020 – ‘stay home, protect the NHS, save lives’.
Asked if he thought the target of vaccinating more than 13million people over the next seven weeks was possible, Professor Whitty said it was ‘realistic but not easy’.
But the medic also delivered a grim message that ‘some’ restrictions could still be needed next winter, as the virus was likely to be in regular circulation like flu.
Surging numbers of infections mean that more people will inevitable end up in hospital and the NHS has warned it is heading towards some of the toughest weeks on record as patient numbers continue to soar.
Professor Chris Whitty warned this week that there is a ‘material risk’ the NHS could be overwhelmed within weeks.
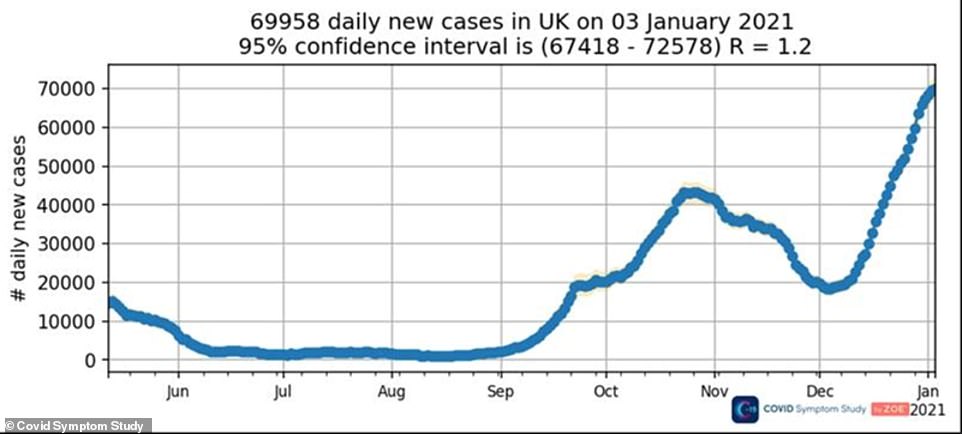
The Covid Symptom Study, which uses reports from around one million people who have the app on their phones, showed that cases have been surging non-stop since the effects of England’s second lockdown wore off in early December
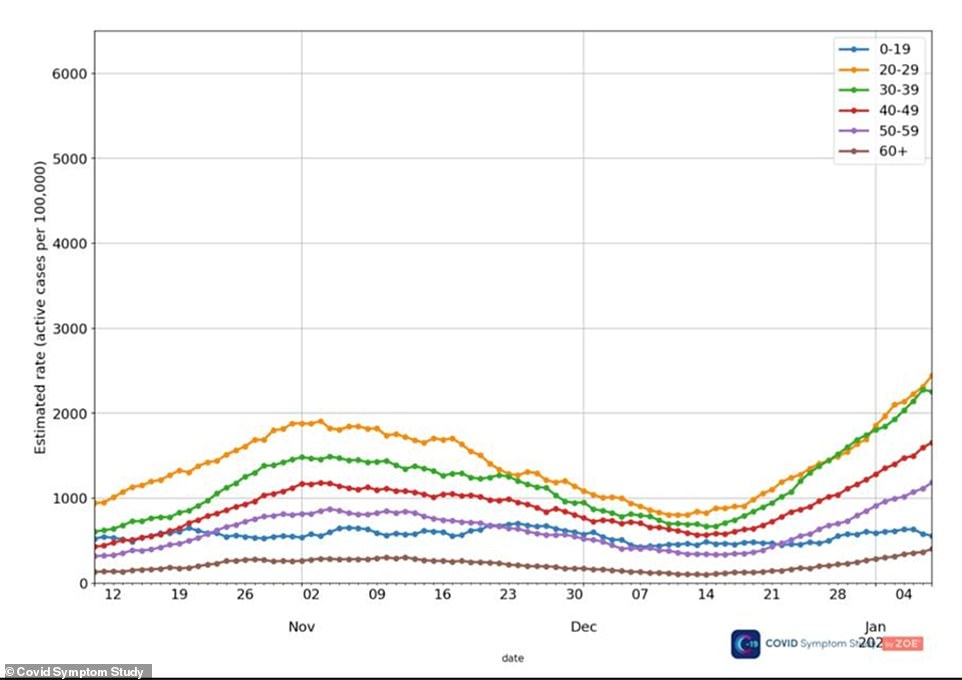
A breakdown of coronavirus cases by age group shows that infections are rising in most age groups but appear to have started to level off or fall
at the start of this year among people in their 30s (green line) and in children and teenagers (blue)

The Covid Symptom Study app data suggests that coronavirus outbreaks are worst in London and Wales and least bad in Devon, the Humber and Bath and Somerset
London’s hospitals will be overwhelmed by Covid-19 in less than two weeks even in a ‘best’ case scenario, according to health chiefs.
Medical director at NHS London, Vin Diwakar, provided the worrying analysis to medical directors of the capital’s hospital trusts over a Zoom call yesterday afternoon.
Even if coronavirus patients grew at the lowest likely rate and capacity is increased – including opening the Nightingale – the NHS would still be short 2,000 general, acute and ICU beds by January 19, the HSJ reported.
Three scenarios are laid out for both G&A and intensive care – ‘best’, ‘average’ and ‘worse’. These account for the impact of four per cent daily growth, five per cent growth and six per cent growth, respectively.
The briefing shows that the NHS in London had just 46 spare ICU beds on January, which is 3 per cent of its overall capacity. Over 70 per cent of its critical beds were taken up by people with Covid.
On the same date there were just spare 720 general and acute beds, 5 per cent of its total, and more than 40 per cent were in use by infected patients.
Hospitals may have to start transferring patients to care homes if coronavirus keeps piling pressure on their wards, a senior health official has warned.
Chris Hopson, chief of healthcare union NHS Providers, warned that some hospitals are almost full already and looking for beds elsewhere for their patients.
‘They know there is some spare capacity in the care and nursing sector,’ he said. ‘They’re in the middle of conversations with care and nursing home colleagues to see if they can access that capacity.
‘It’s literally leaving no stone unturned to maximise every single piece of capacity that we’ve got, in those areas under pressure.’
If care homes are turned into overflow wards for hospitals it is likely only non-Covid patients would be sent to them, following uproar over a Government policy in the first wave which saw people recovering from coronavirus sent into care homes where they were feared to have triggered killer outbreaks.
On BBC Radio 4 yesterday morning Mr Hopson said the situation is ‘really escalating very quickly’.
‘We’ve seen 5,000 new patients in hospital beds with Covid-19 over the last week – that’s 10 full hospitals worth of new Covid patients in just seven days so there’s a really big challenge.’
He said the Nightingales hadn’t been utilised – except in Manchester and Exeter – because they required staffing, snatching vital doctors and nurses away from overstretched wards and emergency units.
‘It’s better if we can access any spare capacity in the nursing home sector because its got staff there,’ he said.
‘We all recognise that if we’re going to do that then we really need to help care and nursing home.
‘So, for example, if we’re going to discharge patients who need consistent access to high quality therapy we’re going to need to ensure that our community services can provide that support.
‘We also know if we’re going to discharge patients that are perhaps slightly more higher levels of acuity than normal we’re going to have to provide extra nursing support.
‘The issue is we’re now at a point where unless we can access this capacity, we’re not going to be able to treat the patients that we need to treat in the NHS.’
But care home bosses are against the idea and warned it would be a ‘grave mistake’, risking triggering
outbreaks among extremely vulnerable residents and adding to already ‘phenomenal’ pressure that homes are facing.
Vic Rayner, chief executive of the National Care Forum, which represents not-for-profit care homes, said today: ‘It would be a grave mistake to discharge large numbers of Covid-19 positive people to care and nursing homes, particularly with the new variant of the vaccine being so virulent.
‘Hospital patients must not be discharged to care homes without a cleared test result and there must not be pressure for care homes to take patients who are Covid-19 positive if they are not either established as a designated scheme, or have suitable arrangements in place.
‘The crisis and pressure in the hospital sector is mirrored in the care and nursing home sector where we are already seeing testing and widespread community transmission causing rapid and unpredictable staffing shortfalls, adding phenomenal pressure to an exhausted and stretched workforce.
‘Calls to protect the NHS must not ignore the massive potential impact on those living and working within care.’