Top surgeon fears cancer surgeries could be cancelled AGAIN unless No10 can curb spread of Covid
A top surgeon today raised fears cancer surgeries may be axed in the coming days, unless the national lockdown swiftly curbs the spread of coronavirus.
Professor Neil Mortensen, the president of the Royal College of Surgeons, rang alarm bells today after warning the situation in hospitals is getting ‘much worse’, and escalating faster than the ‘slow-motion car crash’ he previously predicted.
Adding to mounting warnings, he said other non-Covid treatments such as knee replacements may also be put on hold because of escalating Covid admissions.
Dr Claudia Paoloni, the chairman of the Hospital Consultants and Specialists Association, echoed his warning today saying the risk of hospitals becoming overwhelmed in the next few weeks is ‘very, very high’.
King’s College hospital in south London has already called off all ‘priority 2’ cancer operations, procedures which specialists have judged to be urgent and need to be done within 28 days of a decision to undertake them.
It is feared other hospitals in the country may face the same difficult decision in the coming days if admissions don’t start to fall.
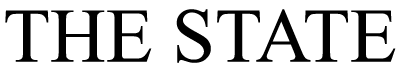
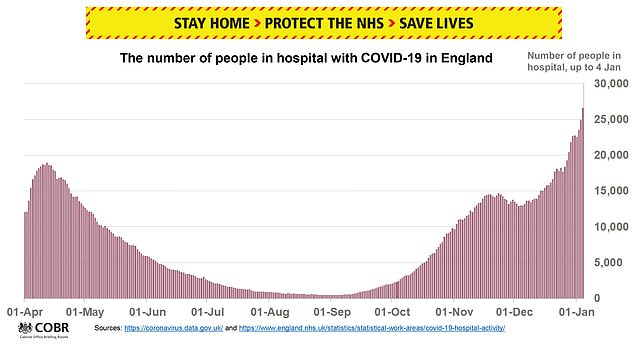
Healthcare services are already 40 per cent busier than during the first wave in April, Boris Johnson has said, as doctors liken working for the NHS to being in a warzone.
It comes after Britain’s chief medical officers warned there was a ‘material risk’ of the NHS being overwhelmed in the next 21 days.

A top surgeon has warned those waiting for operations to treat cancer could have their surgery axed due to spiralling admissions. Above are ambulance workers outside the Royal London Hospital on January 3
Professor Mortensen told Times Radio: ‘My colleagues in London doing ward rounds, for example, report that there are problems with staff numbers on the wards, staff numbers in theatres.
‘And then of course if you need to go to the intensive care unit, if the intensive care unit is full of Covid patients there’s no room for you.
‘So it’s a really serious situation and, obviously, the less-priority operations have already stopped in many places – hips, knees, ENT (ear nose and throat) procedures.
‘We’re now concerned about operations like cancer surgeries being cancelled or postponed because there just isn’t the capacity to be able to manage them.’
He added: ‘I think if you have a delayed operation for cancer that may have an effect.
‘If you come in from a road traffic accident and you’re seriously ill, and you need to go to an intensive care unit afterwards and there is no intensive care unit, that’s going to have seri
ous consequences.
‘And that’s why everybody is so concerned right now that we are properly locked down, that we’re as far as we possibly can reducing the transmission of the virus, and making it possible for what facilities we do have to carry on working effectively to keep people alive.’
Warning that those waiting for treatments for other illnesses also faced seeing their procedures cut, Professor Mortensen added: ‘There needs to be space in our hospitals for us to deal with all the other things – the heart attacks or strokes, the cancer surgeries and emergency surgery.
‘We have to be able to keep capacity to do those. And if we don’t reduce the transmission of the virus, there won’t be that capacity.’
When asked whether the NHS will be able to return to normal business by late spring, he added: ‘I’m afraid I’m one of the pessimists I think this is going to drag on a bit.
‘I think that we’re really not going to be any bit in any better shape (until) summer I’m afraid.

Professor Neil Mortensen, president of the royal college of surgeons
‘I think it’s going to take a long time. This is a very, very, very serious situation.
‘There’ll be an enormous backlog of elective surgeries, and we may have backlogs of some more urgent surgeries to get through as well so it’s going to be a long tough, hard winter and spring.’
Dr Paoloni warned on BBC Radio 4’s Today programme: ‘We’re now in a situation where the risk of overwhelming the NHS at this point, over the next few weeks, is very, very high.
‘We are very much hoping that this (lockdown) will avert an overwhelming.’
Asked what hospitals being overwhelmed could look like, she said: ‘What you see in London, on the news or in the papers, with ambulances lined up, unable to load their patients into Accident and Emergencies, could happen in every hospital throughout this country, which means that anyone with any condition may not be able to access the care that they need.’
King’s College hospitals decision to postpone cancer operations has led to fears among staff that some of the affected patients may see their cancers spread of become inoperable, reports The Guardian.
‘It’s important to do these cancer cases within four weeks because they’re urgent,’ one member of staff told the newspaper.
‘If you put cancer surgery off for more than four weeks, that cancer can spread. (The delay can mean that) surgery may become inappropriate, because surgery can no longer get rid of the cancer, and thus the patient’s outcome may be worse.’
King’s has confirmed it has cancelled priority 2 cancer operations.
A spokesman said: ‘Due to the large increase in patients being admitted with Covid-19, including those requiring intensive care, we have taken the difficult decision to postpone all elective procedures, with the exception of cases where a delay would cause immediate harm.’

Boris Johnson pictured visiting the Chase Farm Hospital in London yesterday
Britain’s chief medical officers have warned parts of the NHS are already under ‘immense pressure’, as Covid-19 cases continue to spiral.
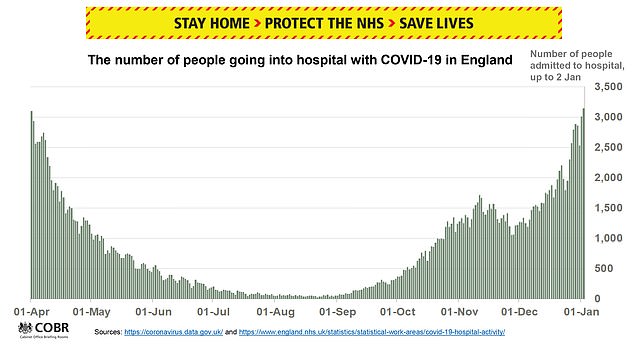
They have raised the alert level to five – its highest – for the first time since the pandemic began, meaning ‘transmission is rising exponentially’ and healthcare services may be overwhelmed.
In a letter written by the UK’s four CMOs and NHS England’s national medical director Professor Stephen Powis – ahead of Mr Johnson’s address – said: ‘Following advice from the Joint Biosecurity Centre and in the light of the most recent data, the four UK chief medical officers and NHS England medical director recommend that the UK alert level should move from Level 4 to Level 5.
‘Many parts of the health systems in the four nations are already under immense pressure. There are currently very high rates of community transmission, with substantial numbers of Covid patients in hospitals and in intensive care.
‘Cases are rising almost everywhere, in much of the country driven by the new more transmissible variant. We are not confident that the NHS can handle a further sustained rise in cases and without further action there is a material risk of the NHS in several areas being overwhelmed over the next 21 days.
‘Although the NHS is under immense pressure, significant changes have been made so people can still receive lifesaving treatment.
‘It is absolutely critical that people still come forward for emergency care. If you require non-urgent medical attention, please contact your GP or call NHS 111.’
The Prime Minister sent England into its third lockdown yesterday, with shutdowns also in place in Scotland, Wales and Northern Ireland.
As many as 80,000 positive cases were recorded on December 29 alone, thought to have been key in the Prime Minister’s decision to once again draw the curtains on society.