Care workers with Covid told to stay in work as NHS tries to put patients from hospitals into homes
Care home staff have been told to go into work despite testing positive for coronavirus, an alarming new report has revealed today.
In the past fortnight inspectors have flagged more than a dozen care homes over problems with infection control.
The Care Quality Commission has reportedly warned at least 14 homes about flaws, including telling workers with Covid to work due to staff shortages, the Guardian reported.
This comes as the NHS makes plans to commandeer spare care beds across the country to help release pressure on hospitals as their wards fill up with Covid patients.
National Care Association chairwoman Nadra Ahmed told BBC Radio 4’s Today programme: ‘There’s no way that providers can go back to April when we were told everything was OK and people were being discharged out of hospitals. Of course we want to help the NHS if we can, but we have to do that safely.
‘The only way that can be safely done is if we’re absolutely clear that the person is no longer shedding the virus and bringing it into the care service.
‘We also have to remember that care homes are also struggling with staffing. The risk to the sector is enormous if we don’t do this in a safe manner.’

Hospitals across England are seeing more coronavirus patients than they did in the first wave in 2020 (Pictured: Staff in an intensive care ward in St George’s Hospital in London)

A medic works with a patient in the ICU (Intensive Care Unit) in St George’s Hospital in Tooting, south-west London
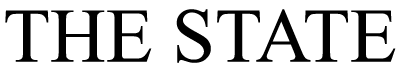
Some hospitals are approaching breaking point, and preparing to turn to care homes for help, the chief executive of NHS Providers has said. The number of Covid-19 patients in hospital had surged past 30,000 by January 4, NHS data reveals
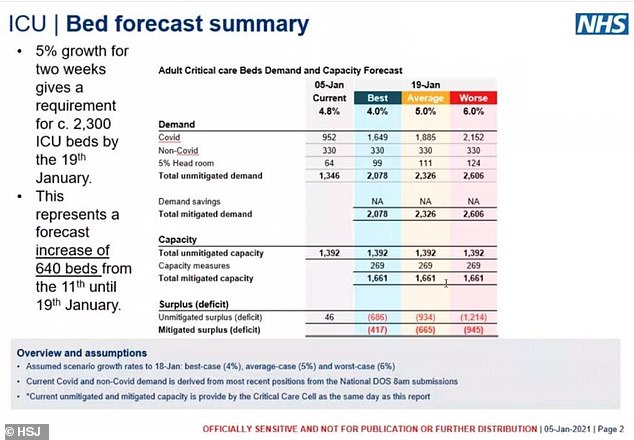
Chris Hopson, chief of healthcare union NHS Providers, said yesterday that some hospitals are almost full already and looking for beds elsewhere for their patients.
But Ms Ahmed warned that many care home providers are operating with their normal insurance in place – meaning that if they take a Covid-positive patient, it would nullify their insurance.
Campaigners warn this may lead to a repeat of the ‘disaster’ last spring when infectious patients were sent to care homes and tens of thousands of deaths resulted.
Charities and care leaders say they have a ‘horrible sense of déjà-vu’ and it would be a ‘grave mistake’.
But NHS bosses say they are running out of beds due to soaring virus admissions and desperately need to offload patients to the care sector.
Ms Ahmed told Radio 4 today: ‘I don’t know who Chris has been speaking to, but the providers we represent are all very co
ncerned about the risk of bringing the virus into their services.
‘We are not funded properly and that’s not being looked at.
‘A lot of providers are practising with the normal insurance in place but Covid is excluded so if we take people who are positive into our services, it could nullify our insurance and the government hasn’t moved forward to do anything about that for our sector, but they did it for the NHS.
‘So surely if the NHS is looking to move people into social care settings then that has to be underwritten as a precursor to anything.
‘We need to be very clear – isolation in care home is in place. But there is so much that needs to be done before we can go into the role of taking hospital patients.’
If care homes are turned into overflow wards for hospitals it is likely only non-Covid patients would be sent to them, following uproar over a Government policy in the first wave which saw people recovering from coronavirus sent into care homes where they were feared to have triggered killer outbreaks.

Chris Hopson, chief executive of NHS Providers, warned of spiralling admissions
More than 30,000 people are currently in hospital with Covid across the UK and the number is expected to soar after more than 300,000 people tested positive in the last week of December.
This was up 27 per cent in a week and towers above the worst figure of 21,700 seen in April 2020.
Chris Hopson warned yesterday: ‘We are now reaching the point where hospital beds are full, community beds are full, and community at-home services are also full.
‘What trust leaders are now trying to do is [use] spare capacity in the care and nursing home sector.
‘They are in the middle of conversations with their care and nursing home colleagues to see if they can access that capacity.’
Mr Hopson said care homes were better placed to accept patients than Nightingale hospitals because they had more staff. He called on the Government to create financial incentives for care homes to take NHS patients.
He added: ‘There is, of course, no question of using this capacity for patients who could introduce Covid-19 infection risk into care homes or for patients requiring complex or specialist hospital care.’

A staff nurse treats patient Peter Watts, 64, in the emergency department at St George’s Hospital in Tooting
MailOnline has contacted NHS England to ask how care homes may be utilised to help take the pressure off central hospitals.
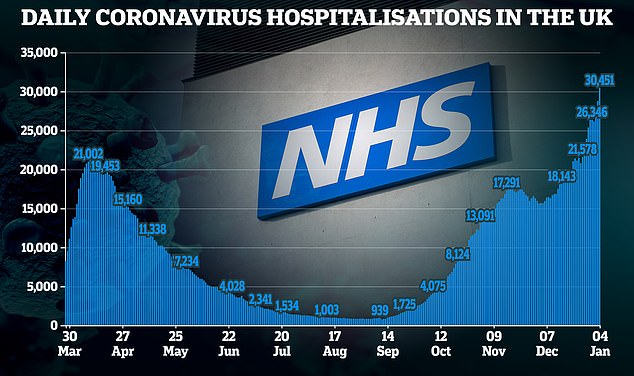
Intensive care patients are already being moved from the hardest hit regions to those where there is spare capacity.
Some doctors are currently considering moving the most critically ill from London and the South East to as far afield as Yorkshire and the South West.
The President of the Intensive Care Society, Dr Stephen Webb, said yesterday around 10 intensive care patients were already being shifted every day.
Most of these are moved from and to hospitals within the same regions, he said, but a small number may be moved between regions.

A patient is prepared for transfer from the Acute Dependency Unit to the ICU (Intensive Care Unit) at St George’s Hospital

At St George’s a surge in coronavirus patients has meant the number of intensive care beds had to be doubled from 60 to 120

Staff sickness due to coronavirus and self-isolation means doctors, nurses and healthcare assistances face demanding shift patterns and exhausting work looking after critically ill Covid-19 patients (Pictured: Staff in St George’s Hospital)

There were 30,451 people in hospital with Covid-19 as of January 4, with 2,645 on ventilators in intensive care
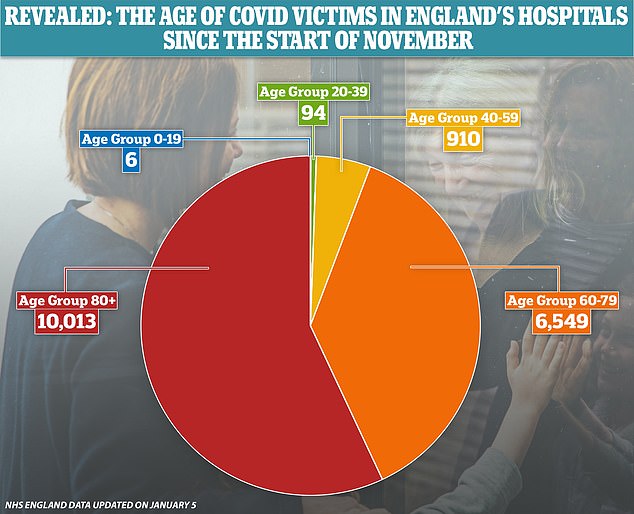
NHS statistics show that it is rare for people under the age of 40 to die of Covid-19, with 100 of the 17,572 fatalities in November and December in that age group

Nurses and doctors work on wards at University College Hospital, London, pictured above
Normally, it is rare for intensive care patients to be moved between hospitals.
Dr Webb, who also works in the East of England, said: ‘The problem with sending patients to the North is that those units were really badly affected earlier in this wave, and they could be hit with the new variant. It’s a very tricky situation.
‘If the virus continues as it is, I’m much more fearful we may get to saturation point for ICUs, but we have still got a bit of time. We do have capacity in other parts of the country, but not a lot.
‘Currently, in the East of England, South East and London, many intensive care units are already saturated. This is where we’re seeing daily export of patients. but at the moment this is mainly locally.
‘So it may be a few miles down the road between London hospitals. We try to avoid moving patients and we always try to move the least sick of our ICU patients. They are transferred using all the equipment needed to keep them alive, accompanied by an ICU doctor and a nurse.’